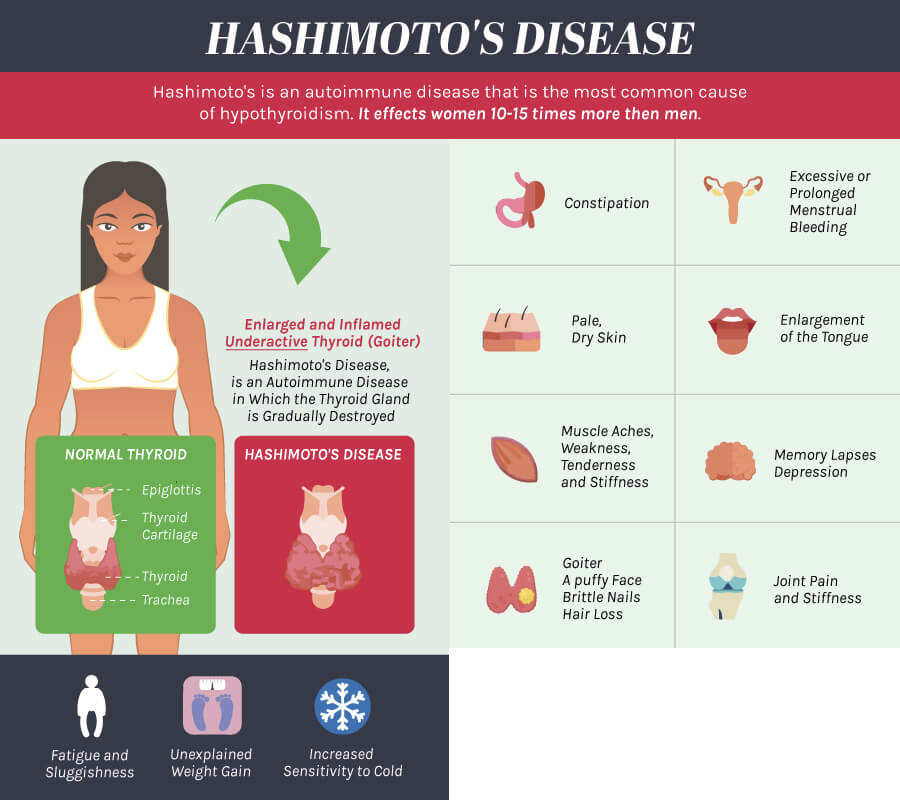
is the most common thyroid disorder affecting up to 15% of women and one quarter as many men. It is an autoimmune condition that interferes with thyroid function. In the case of Hashimoto’s thyroiditis, immune cells mistakenly attack healthy thyroid tissue,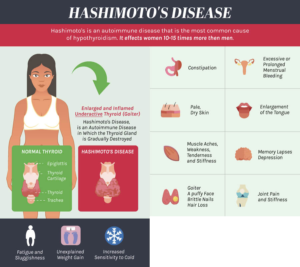 causing inflammation of the thyroid. This inflammation, also known as chronic lymphocytic thyroiditis, often leads to an under active thyroid gland (hypothyroidism). Initial symptoms can be mild, progressing slowly over time as the chronic thyroid damage leads to a drop in thyroid hormone levels in the patients blood. Thyroid hormones control how the body uses energy, and can have a broad range of symptoms as thyroid hormones affect nearly every organ in the body. A combination of factors including heredity, sex and age may determine the patient’s likelihood of developing the disorder.
causing inflammation of the thyroid. This inflammation, also known as chronic lymphocytic thyroiditis, often leads to an under active thyroid gland (hypothyroidism). Initial symptoms can be mild, progressing slowly over time as the chronic thyroid damage leads to a drop in thyroid hormone levels in the patients blood. Thyroid hormones control how the body uses energy, and can have a broad range of symptoms as thyroid hormones affect nearly every organ in the body. A combination of factors including heredity, sex and age may determine the patient’s likelihood of developing the disorder.
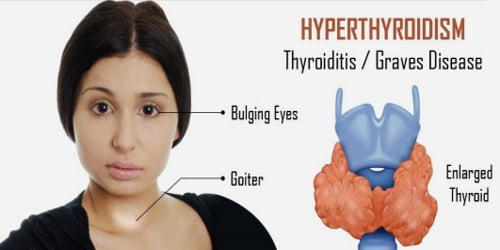
Graves’ disease is a autoimmune illness that causes the thyroid gland to overactive, producing too much thyroid hormone, called hyperthyroidism. Normally, thyroid function is regulated by a hormone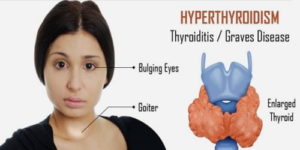 released by the pituatary gland at the base of the brain. The antibody associated with Graves’ disease, thyrotropin receptor antibody (TRAb), acts like the regulatory pituitary hormone. Effectively TRAb overrides the normal regulation of the thyroid, causing an overproduction of thyroid hormones. The progression of the disease varies, in some cases it may even present an alternating pattern of relapse and remission. Left untreated Graves Disease can cause eye changes, and complications such as heart disease and bone loss.
released by the pituatary gland at the base of the brain. The antibody associated with Graves’ disease, thyrotropin receptor antibody (TRAb), acts like the regulatory pituitary hormone. Effectively TRAb overrides the normal regulation of the thyroid, causing an overproduction of thyroid hormones. The progression of the disease varies, in some cases it may even present an alternating pattern of relapse and remission. Left untreated Graves Disease can cause eye changes, and complications such as heart disease and bone loss.
is a condition in which the thyroid gland is overactive and makes excessive amounts of thyroid hormone. The thyroid gland is an organ located in the front of your neck and releases hormones that control your metabolism (the way your body uses energy), breathing, heart rate, nervous system, weight, body temperature, and many other functions in the body. Hyperthyroidism increases metabolism, and can cause disturbed sleep, palpitations, tremor, sweats, weight loss, and increased frequency of bowel movements. It may result from Graves’ disease, from an autonomously functioning thyroid nodule, or it may be a temporary result of subacute thyroiditis.
is a condition in which the thyroid gland is under active and makes inadequate amounts of thyroid hormone. The thyroid gland is an organ located in the front of your neck and releases hormones that control your metabolism (the way your body uses energy), breathing, heart rate, nervous system, weight, body temperature, and many other functions in the body. Hypothyroidism causes a slowing of metabolism, with fatigue, weight gain, dry skin, hair loss, brittle nails, and constipation. It most frequently results from Hashimoto’s disease.
Thyroid nodules, or growths in the thyroid, are very frequent, affecting up to half of people by the age of 60. Many of them are benign, but some are malignant, and may require a needle biopsy for diagnosis
is a case where the typical thyroid nodule is malignant, and replicate or spread to other tissues and organs. There are 4 main types of thyroid cancer, and some are more common than others.
Thyroid cancers vary in aggressiveness by type:
and/or mixed papillary/follicular thyroid cancer (85%) grows slowly and spreads locally.
and/or Hurthle cell thyroid cancer (10%) is more likely to metastasize to distant sites than Papillary.
thyroid cancer (3%) is uncommon and more aggressive than papillary or follicular types.
thyroid cancer (1%) is rare and more aggressive than papillary or follicular types.
Fast and accurate diagnosis is critical to treatment and management of thyroid cancers.
can involve either abnormalities within the uterus (like uterine fibroids) or external conditions that are more difficult to diagnose. Irregular or absent periods can result from PCOS, or diseases of the thyroid, adrenals or pituitary gland. It can also be caused by systemic illnesses.
can be caused by increased male hormone levels originating from the ovaries or adrenal  glands, or by increased sensitivity to seemingly normal levels of hormones. Skin specialists and primary care doctors often recommend that women with acne that is resistant to antibiotics see an endocrinologist. An endocrinologist will work to confirm the acne is not a symptom of polycystic ovary syndrome, a common disorder in young women.
glands, or by increased sensitivity to seemingly normal levels of hormones. Skin specialists and primary care doctors often recommend that women with acne that is resistant to antibiotics see an endocrinologist. An endocrinologist will work to confirm the acne is not a symptom of polycystic ovary syndrome, a common disorder in young women.
is hair loss that is the result of exposure to male hormones in a genetically susceptible person. Scalp hair loss can be caused by problems with the ovaries, adrenals, thyroid, or pituitary gland. There are treatments available after confirming the hair loss is a hormonal issue. Careful evaluation is required as hair loss can also result from nutritional deficiencies, systemic illnesses, and medication effects.
susceptible person. Scalp hair loss can be caused by problems with the ovaries, adrenals, thyroid, or pituitary gland. There are treatments available after confirming the hair loss is a hormonal issue. Careful evaluation is required as hair loss can also result from nutritional deficiencies, systemic illnesses, and medication effects.
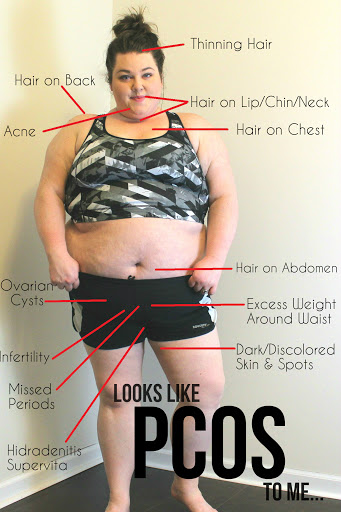
is caused by an imbalance of reproductive hormones, creating problems 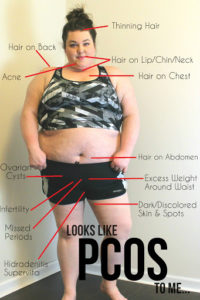 in the ovaries. The ovaries make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be. PCOS can cause irregular or absent periods, increased male hormone effects such as acne, hirsutism, and scalp hair loss, and increased weight.
in the ovaries. The ovaries make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be. PCOS can cause irregular or absent periods, increased male hormone effects such as acne, hirsutism, and scalp hair loss, and increased weight.
Sexual Dysfunction is a condition in which there is a low desire to engage in sexual activity. Treatment of sexual dysfunction depends on the cause of the condition. Low desire and sexual dysfunction can be caused by problems with the testicles, adrenals, thyroid, or pituitary glands. It can also result from systemic illnesses such as diabetes, kidney and liver disease, infections, and medication effects. For some men, adopting a healthier lifestyle, such as exercising regularly, eating a healthy diet, getting enough sleep, reducing stress, and/or limiting alcohol, can help resolve the problem. Common causes of low libido include:
Medications (SSRI antidepressants; medications that reduce testosterone levels, such as those taken for prostate cancer)
Excessive alcohol use or recreational drug use
Systemic illness (such as chronic lung, heart, kidney and liver failure, cancer)
Low testosterone (male hypogonadism)
Depression
Relationship problems
Erectile dysfunction (ED)
Erectile dysfunction (ED), or Impotence, is the inability to consistently initiate or keep an erection long enough to have satisfactory sex. Erectile dysfunction (ED) is a disorder with multiple etiologies, which may be psychogenic and/or organic in origin. Among the organic causes of ED are diseases of the endocrine system, including hormone imbalance, Low testosterone, high prolactin, diabetes mellitus, and abnormal thyroid hormone levels.
Among the organic causes of ED are diseases of the endocrine system, including hormone imbalance, Low testosterone, high prolactin, diabetes mellitus, and abnormal thyroid hormone levels.
also called Low Testosterone, is a condition where the testes produce an abnormally low level of testosterone. Although testosterone levels never reach zero (as estrogen levels do in women during menopause), low testosterone levels men to experience symptoms such as fatigue, low sex drive, and loss of muscle mass. Hypogonadism, can either be primary, resulting from testicular damage, or secondary, caused by pituitary or hypothalamic disease.
Primary Hypogonadism is also known as primary testicular failure, and it is caused by a problem in the testicles. These problems can include:
Secondary Hypogonadism is caused by a problem with the pituitary or hypothalamus glands. Those are glands that give a signal to the testicles to make testosterone, so if something affects them, testosterone production can be affected. Conditions that can cause secondary hypogonadism include:
is a condition where the hard, dense material that forms bone becomes porous, and bones become weaker and subject to fracture. Osteoporosis takes place across years, with no symptoms, gradually progressing to the point where a fracture is imminent. Osteoporosis, with increased risk of fractures and skeletal deformity, can result from hormonal problems such as decreased ovarian or testicular function, or disease of the parathyroid glands, adrenals, thyroid, or pituitary gland. It can also occur because of nutritional deficiency such as inadequate intake of calcium and vitamin D, or an effect of medications such as steroids or chemotherapy agents.
and bones become weaker and subject to fracture. Osteoporosis takes place across years, with no symptoms, gradually progressing to the point where a fracture is imminent. Osteoporosis, with increased risk of fractures and skeletal deformity, can result from hormonal problems such as decreased ovarian or testicular function, or disease of the parathyroid glands, adrenals, thyroid, or pituitary gland. It can also occur because of nutritional deficiency such as inadequate intake of calcium and vitamin D, or an effect of medications such as steroids or chemotherapy agents.
While the reasons for hair loss vary immensely, most of our patients achieve impressive results by combining PRP for hair restoration with hormone optimization. As your body ages, hormone levels decline. As a result, your metabolism slows down – which slows down hair growth. While your hair growth slows, the hair loss cycle does not slow down. Hence, this brings about thinning hair – which concerns our patient.
achieve impressive results by combining PRP for hair restoration with hormone optimization. As your body ages, hormone levels decline. As a result, your metabolism slows down – which slows down hair growth. While your hair growth slows, the hair loss cycle does not slow down. Hence, this brings about thinning hair – which concerns our patient.
is a condition that increases neuromuscular irritability manifested as numbness and tingling, particularly of the distal extremities, however, most patients are asymptomatic. Longstanding hypocalcemia due to hypoparathyroidism can result in calcification of the basal ganglia and other intracerebral calcifications, cataracts, dermatological manifestations including dry, puffy skin, and coarse, brittle and sparse hair.
is a condition where the parathyroid produces too much hormone resulting in bone releasing calcium into the blood. This released calcium is a cause for osteoporosis and the elevated blood calcium leads to increased urinary excretion of calcium causing kidney stones. There can also be muscle, bone, and joint pain, and impairment of cognitive function.
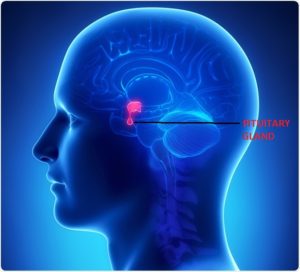
is caused by a pituitary tumor that produces excess growth hormone (GH). It most commonly affects middle-aged adults and can result in serious illnesses or premature death.
Pituitary Adenoma is a growth or tumor on the pituitary that can put pressure on nearby structures, such as the nerves that connect the eyes to the brain, and cause symptoms. A large adenoma can also obstruct normal pituitary cells and keep them from working properly, leading to a condition called hypopituitarism. This condition can cause low blood pressure, tiredness, and changes in your sex drive and function. It can also make you feel less able to manage stress.
and cause symptoms. A large adenoma can also obstruct normal pituitary cells and keep them from working properly, leading to a condition called hypopituitarism. This condition can cause low blood pressure, tiredness, and changes in your sex drive and function. It can also make you feel less able to manage stress.
Hyperpituitarism is a condition due to the primary hypersecretion of pituitary hormones, it typically results from a pituitary adenoma
Prolactinomas are benign tumors of the pituitary gland that produce excessive amounts of the hormone prolactin. Prolactinomas are most common pituitary disorder, appearing in 50% of cases. In women, excess prolactin causes irregular or absent periods, inappropriate milk production, and infertility. In men, excess prolactin can cause sexual dysfunction and infertility. Symptoms can result from too much prolactin in the blood (hyperprolactinemia) or pressure from the tumor on surrounding tissues (if the tumor is large).
sexual dysfunction and infertility. Symptoms can result from too much prolactin in the blood (hyperprolactinemia) or pressure from the tumor on surrounding tissues (if the tumor is large).
Hypopituitarism and Panhypopituitarism, If the pituitary is not producing one or more of these hormones, the condition is called hypopituitarism. If all the hormones produced by the anterior pituitary are decreased, the condition is called panhypopituitarism. Hypopituitarism is most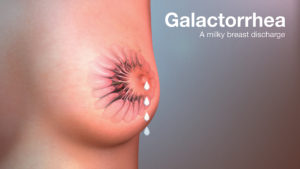 often caused by large benign tumors of the pituitary gland, or of the brain in the region of the hypothalamus.
often caused by large benign tumors of the pituitary gland, or of the brain in the region of the hypothalamus.
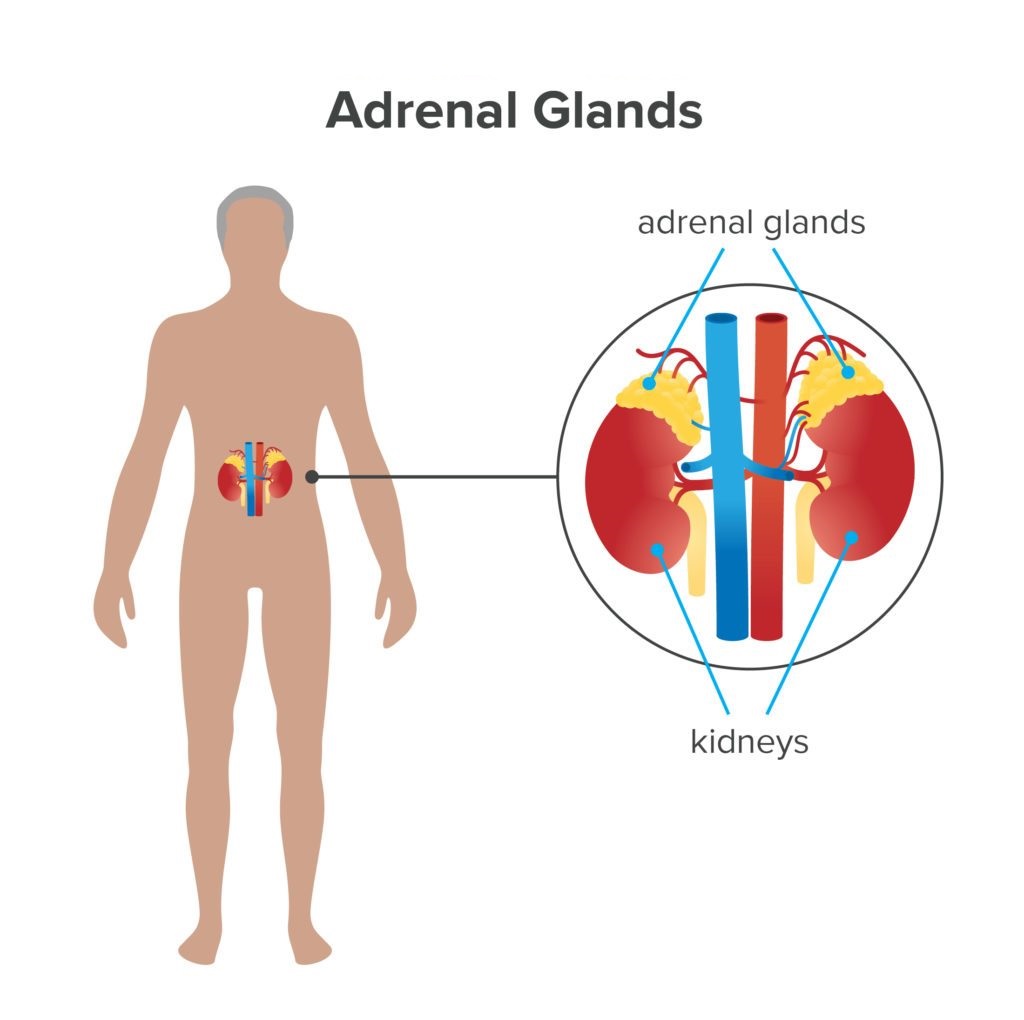
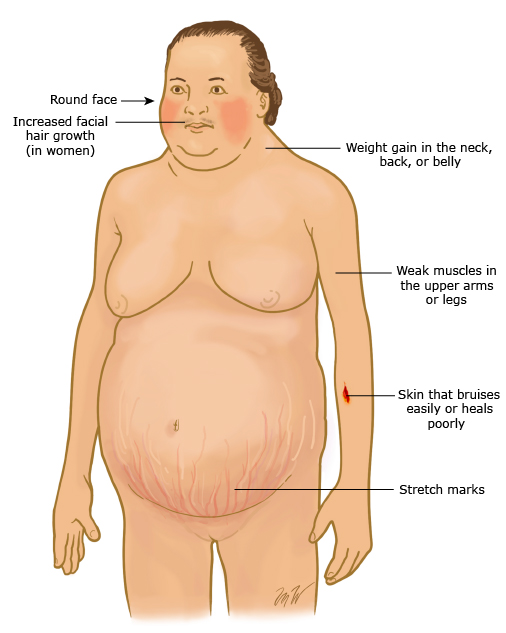
ushing’s Disease refers to a pituitary adenoma that produces excess ACTH,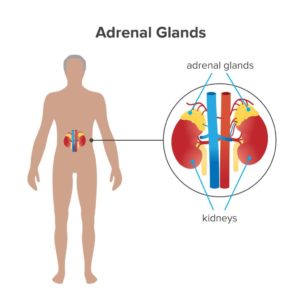 which stimulates cortisol secretion by the adrenal glands located above each kidney. Patients with Cushing’s disease have progressive weight gain, muscle weakness, easy skin bruising, impotence (in men), irregular periods (in women), and depression. Patients also have high blood pressure, diabetes, and osteoporosis. Many of these problems are non-specific.
which stimulates cortisol secretion by the adrenal glands located above each kidney. Patients with Cushing’s disease have progressive weight gain, muscle weakness, easy skin bruising, impotence (in men), irregular periods (in women), and depression. Patients also have high blood pressure, diabetes, and osteoporosis. Many of these problems are non-specific.
is a disorder in which the adrenal glands do not produce enough of the hormones cortisol and aldosterone. Addison’s disease is caused by an autoimmune 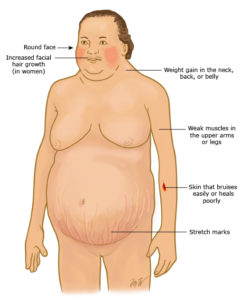 response, in which the body’s immune system assaults its own organs and tissues. Cortisol helps the body respond to stress, including the stress of illness, injury, or surgery. It also helps maintain blood pressure, heart function, the immune system, and blood glucose (sugar) levels. Aldosterone affects the balance of sodium and potassium in the blood, which in turn controls the amount of fluid the kidneys remove as urine, which affects blood volume and blood pressure
response, in which the body’s immune system assaults its own organs and tissues. Cortisol helps the body respond to stress, including the stress of illness, injury, or surgery. It also helps maintain blood pressure, heart function, the immune system, and blood glucose (sugar) levels. Aldosterone affects the balance of sodium and potassium in the blood, which in turn controls the amount of fluid the kidneys remove as urine, which affects blood volume and blood pressure
Born Again Doctor Medical Center diagnose lipid disorders with blood 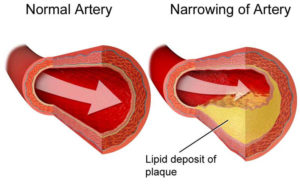 tests and sometimes with additional imaging tests.
tests and sometimes with additional imaging tests.
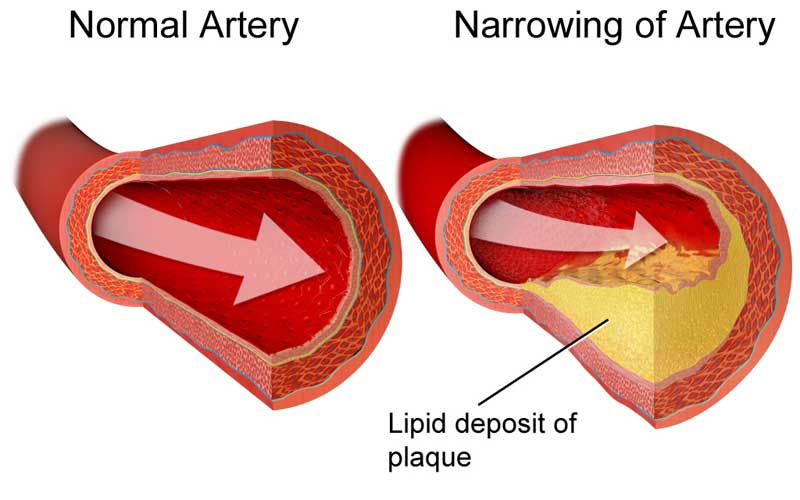
Lipids are waxy fats in the blood that are essential to a wide range of bodily functions. Cholesterol and triglycerides are two kinds of lipids.
Cholesterol is present in the cells of the body, and is a dietary component of non-plant foods. Triglycerides are also in the cells and in dietary fat, such as the white fat in meat, oils, and dairy products. The liver also produces cholesterol and triglycerides.
When the blood contains amounts of these substances that are outside of the healthy range—either too high or too low—this is known as a lipid disorder. People who have a high amount of certain lipids are at increased risk of developing cardiovascular disease.
Low-Density Lipoprotein
Low-density lipoprotein, known as LDL, or “bad,” cholesterol, is one of the most important components of your lipid profile. It circulates through your bloodstream and deposits cholesterol in your arteries. The cholesterol can accumulate and form plaques, which can lead to blockages that may cause a heart attack or stroke. Reducing your LDL through lifestyle changes and medications can help lower your risk.
High-density lipoprotein, or HDL—the “good” cholesterol—may help remove cholesterol from the body. A high level of HDL is associated with a reduced risk of cardiovascular disease. HDL levels are primarily influenced by genetic factors, but lifestyle changes such as tobacco cessation, weight loss, and exercise may be able to help you raise HDL levels.
Triglycerides are fats that come from foods you’ve eaten and are present in your body’s cells. They are produced by the liver and fat tissue, especially when you consume excess calories, particularly from sugars and starches. The body carries triglycerides to tissues, where they provide energy or are stored, especially in fat tissue.
High levels of triglycerides have been linked to heart disease, as well as insulin resistance, type 2 diabetes, and obesity. Very high levels can also cause pancreatitis, an inflammation of the pancreas. Lifestyle changes, such as exercise, diet, and weight loss, can often help reduce triglyceride levels.
There are several different causes of lipid disorders. One of the most common is a genetic predisposition. Importantly, lifestyle habits can help decrease some of that risk—or worsen it.
A diet high in saturated fat, sugar, and simple carbohydrates can lead to increased lipid levels, especially triglycerides. Having increased belly fat is associated with elevated levels of LDL cholesterol, as well as high blood pressure and the risk of developing diabetes. People with diabetes, especially those who are sedentary, can also have disorders in which triglycerides accumulate in muscles or the liver, rather than being used as energy, which removes them from the body.
Taking certain medications, such as steroids, estrogen used in birth control pills, and certain medications to treat high blood pressure and psychiatric conditions, can increase lipid levels. Certain hormone disorders—including polycystic ovary syndrome (PCOS), hypothyroidism, and type 2 diabetes—can also result in high lipid levels.
A genetic disorder known as familial hypercholesterolemia, which begins in childhood, can cause chronically elevated cholesterol levels throughout a person’s lifetime. Levels may become so high that complications, such as a heart attack and stroke, can occur prematurely—even as early as the preschool years—if a person is not treated from a young age. Family members of people with the condition should be screened for it.
In the early stages of lipid disorders, there are no symptoms. High total cholesterol, high LDL, high triglycerides, and low HDL are often first detected in a routine blood test at an annual checkup. Some people with very high cholesterol and triglyceride levels may develop xanthomas—deposits of cholesterol that appear on the ankles or elbows—but this is not common.
To diagnose a lipid disorder, doctor checks your weight, since being overweight or obese is associated with elevated lipids, cardiovascular disease, and diabetes. Then, he or she may order one or more of the following tests.
Your doctor orders a blood test called a lipid profile. The test, which requires you to fast the night before, measures levels of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides—as well as other markers of health. LDL and HDL cholesterol measured on non-fasting blood are also accurate except in people with increased triglyceride levels, who may need a more specialized lipid test.
If your levels are elevated, your doctor may ask about your family history, diet, exercise habits, and other aspects of your lifestyle. He or she may perform further tests to rule out other causes of elevated lipids, such as thyroid disease, liver disease, kidney disease, and medications.
Lipid testing can give your doctor a sense of which foods you should avoid. If the results indicate that you have high levels of triglycerides, your physician is likely to recommend restricting refined carbohydrates, such as white rice and potatoes, as well as saturated and trans fats.
If your doctor wants to better understand your risk of a heart attack or stroke, and determine whether you might need intensive treatment, he or she may order advanced lipid testing.
During this test, your doctor checks your blood not just for levels of LDL and HDL, but for the number, or concentration, of these lipoproteins and their sizes. Some experts believe that this advanced assessment of lipoproteins is a more accurate predictor of cardiovascular disease then the basic lipid profile.
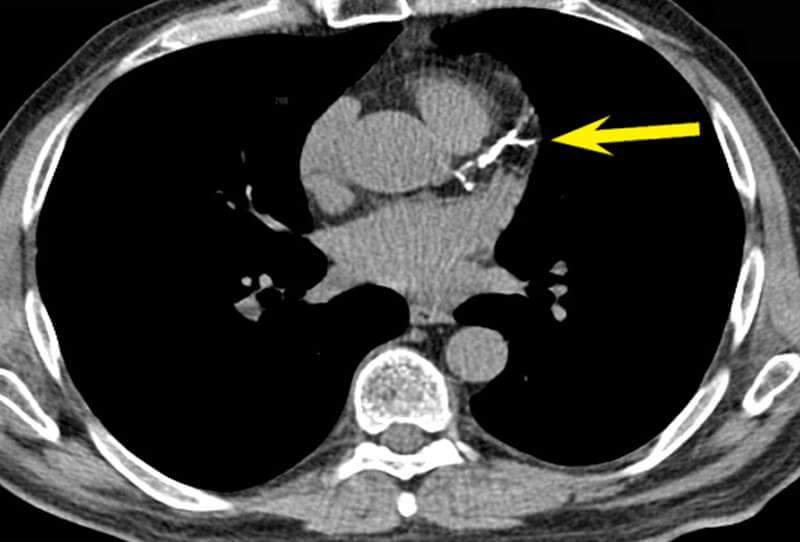
To assess how a lipid disorder is affecting your health and whether 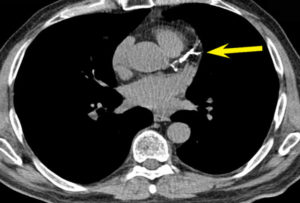 you would benefit from treatment with medication, your doctor may order a coronary calcium score. This test involves a CT scan focused just on the area of the heart, and uses X-rays to assess the amount of calcium in your coronary arteries.
you would benefit from treatment with medication, your doctor may order a coronary calcium score. This test involves a CT scan focused just on the area of the heart, and uses X-rays to assess the amount of calcium in your coronary arteries.
This exam enables your doctor to look for calcium deposits in the walls of your coronary arteries, which are an indication of the buildup of plaque that represents early coronary artery disease. A coronary calcium score has been shown to be an accurate reflection of a person’s risk of cardiovascular disease, and helps your doctor to determine how aggressively to treat a lipid disorder.
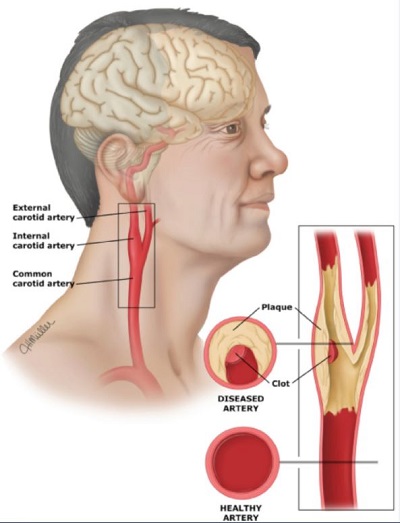
A carotid intima-media thickness test is an ultrasound exam that allows the doctor to measure the amount of plaque in the neck arteries. This measurement gives your doctor an idea of how likely you are to develop cardiovascular disease.
The technician administering the test applies a thick gel to your neck, then moves a handheld device called a transducer up and down your neck. Sound waves bounce off the arteries in the neck, called the carotid arteries, and create images that are transmitted on a computer screen.
The test measures the thickness of the inner and middle layers of the arteries, 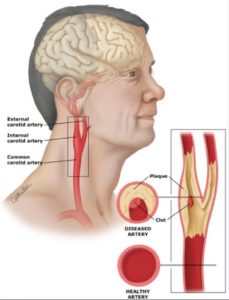 the areas where cholesterol deposits first appear. An increase in the thickness of this region may be associated with higher risk of heart attack and stroke.
the areas where cholesterol deposits first appear. An increase in the thickness of this region may be associated with higher risk of heart attack and stroke.
In addition, the amount of plaque in the neck arteries gives your doctor an idea of how much plaque may be in your coronary arteries. If a person has a large buildup of plaque, he or she may need more aggressive treatment to reduce his or her risk of heart attack and stroke
is the most common thyroid disorder affecting up to 15% of women and one quarter as many men. It is an autoimmune condition that interferes with thyroid function. In the case of Hashimoto’s thyroiditis, immune cells mistakenly attack healthy thyroid tissue, causing inflammation of the thyroid. This inflammation, also known as chronic lymphocytic thyroiditis, often leads to an under active thyroid gland (hypothyroidism). Initial symptoms can be mild, progressing slowly over time as the chronic thyroid damage leads to a drop in thyroid hormone levels in the patients blood. Thyroid hormones control how the body uses energy, and can have a broad range of symptoms as thyroid hormones affect nearly every organ in the body. A combination of factors including heredity, sex and age may determine the patient’s likelihood of developing the disorder.
Graves’ disease is a autoimmune illness that causes the thyroid gland to overactive, producing too much thyroid hormone, called hyperthyroidism. Normally, thyroid function is regulated by a hormone released by the pituatary gland at the base of the brain. The antibody associated with Graves’ disease, thyrotropin receptor antibody (TRAb), acts like the regulatory pituitary hormone. Effectively TRAb overrides the normal regulation of the thyroid, causing an overproduction of thyroid hormones. The progression of the disease varies, in some cases it may even present an alternating pattern of relapse and remission. Left untreated Graves Disease can cause eye changes, and complications such as heart disease and bone loss.
is a condition in which the thyroid gland is overactive and makes excessive amounts of thyroid hormone. The thyroid gland is an organ located in the front of your neck and releases hormones that control your metabolism (the way your body uses energy), breathing, heart rate, nervous system, weight, body temperature, and many other functions in the body. Hyperthyroidism increases metabolism, and can cause disturbed sleep, palpitations, tremor, sweats, weight loss, and increased frequency of bowel movements. It may result from Graves’ disease, from an autonomously functioning thyroid nodule, or it may be a temporary result of subacute thyroiditis.
is a condition in which the thyroid gland is under active and makes inadequate amounts of thyroid hormone. The thyroid gland is an organ located in the front of your neck and releases hormones that control your metabolism (the way your body uses energy), breathing, heart rate, nervous system, weight, body temperature, and many other functions in the body. Hypothyroidism causes a slowing of metabolism, with fatigue, weight gain, dry skin, hair loss, brittle nails, and constipation. It most frequently results from Hashimoto’s disease.
Thyroid nodules, or growths in the thyroid, are very frequent, affecting up to half of people by the age of 60. Many of them are benign, but some are malignant, and may require a needle biopsy for diagnosis.
is a case where the typical thyroid nodule is malignant, and replicate or spread to other tiisues and organs. There are 4 main types of thyroid cancer, and some are more common than others.
Thyroid cancers vary in aggressiveness by type:
– Papillary and/or mixed papillary/follicular thyroid cancer (85%) grows slowly and spreads locally.
– Follicular and/or Hurthle cell thyroid cancer (10%) is more likely to metastasize to distant sites than Papillary.
– Medullary thyroid cancer (3%) is uncommon and more aggressive than papillary or follicular types.
– Anaplastic thyroid cancer (1%) is rare and more aggressive than papillary or follicular types.
Fast and accurate diagnosis is critical to treatment and management of thyroid cancers.

Irregular Periods or Absent Periods can involve either abnormalities within the uterus (like uterine fibroids) or external conditions that are more difficult to diagnose. Irregular or absent periods can result from PCOS, or diseases of the thyroid, adrenals or pituitary gland. It can also be caused by systemic illnesses.
Adult Acne and Hirsutism can be caused by increased male hormone levels originating from the ovaries or adrenal glands, or by increased sensitivity to seemingly normal levels of hormones. Skin specialists and primary care doctors often recommend that women with acne that is resistant to antibiotics see an endocrinologist. An endocrinologist will work to confirm the acne is not a symptom of polycystic ovary syndrome, a common disorder in young women.

(androgenetic alopecia) is hair loss that is the result of exposure to male hormones in a genetically susceptible person. Scalp hair loss can be caused by problems with the ovaries, adrenals, thyroid, or pituitary gland. There are treatments available after confirming the hair loss is a hormonal issue. Careful evaluation is required as hair loss can also result from nutritional deficiencies, systemic illnesses, and medication effects.

is caused by an imbalance of reproductive hormones, creating problems in the ovaries. The ovaries make the egg that is released each month as part of a healthy menstrual cycle. With PCOS, the egg may not develop as it should or it may not be released during ovulation as it should be. PCOS can cause irregular or absent periods, increased male hormone effects such as acne, hirsutism, and scalp hair loss, and increased weight.
is a condition in which there is a low desire to engage in sexual activity. Treatment of sexual dysfunction depends on the cause of the condition. Low desire and sexual dysfunction can be caused by problems with the testicles, adrenals, thyroid, or pituitary glands. It can also result from systemic illnesses such as diabetes, kidney and liver disease, infections, and medication effects. For some men, adopting a healthier lifestyle, such as exercising regularly, eating a healthy diet, getting enough sleep, reducing stress, and/or limiting alcohol, can help resolve the problem. Common causes of low libido include:
Medications (SSRI antidepressants; medications that reduce testosterone levels, such as those taken for prostate cancer)
Excessive alcohol use or recreational drug use
Systemic illness (such as chronic lung, heart, kidney and liver failure, cancer)
Low testosterone (male hypogonadism)

Depression
Relationship problems
Erectile dysfunction (ED)
Erectile dysfunction (ED), or Impotence, is the inability to consistently initiate or keep an erection long enough to have satisfactory sex. Erectile dysfunction (ED) is a disorder with multiple etiologies, which may be psychogenic and/or organic in origin. Among the organic causes of ED are diseases of the endocrine system, including hormone imbalance, Low testosterone, high prolactin, diabetes mellitus, and abnormal thyroid hormone levels.
Hypogonadism also called Low Testosterone, is a condition where the testes produce an abnormally low level of testosterone. Although testosterone levels never reach zero (as estrogen levels do in women during menopause), low testosterone levels men to experience symptoms such as fatigue, low sex drive, and loss of muscle mass. Hypogonadism, can either be primary, resulting from testicular damage, or secondary, caused by pituitary or hypothalamic disease.
Primary Hypogonadism is also known as primary testicular failure, and it is caused by a problem in the testicles. These problems can include:
Secondary Hypogonadism is caused by a problem with the pituitary or hypothalamus glands. Those are glands that give a signal to the testicles to make testosterone, so if something affects them, testosterone production can be affected. Conditions that can cause secondary hypogonadism include:
is a condition where the hard, dense material that forms bone becomes porous, and bones become weaker and subject to fracture. Osteoporosis takes place across years, with no symptoms, gradually progressing to the point where a fracture is imminent. Osteoporosis, with increased risk of fractures and skeletal deformity, can result from hormonal problems such as decreased ovarian or testicular function, or disease of the parathyroid glands, adrenals, thyroid, or pituitary gland. It can also occur because of nutritional deficiency such as inadequate intake of calcium and vitamin D, or an effect of medications such as steroids or chemotherapy agents.
Hypocalcemia (elemental calcium) is a condition that increases neuromuscular irritability manifested as numbness and tingling, particularly of the distal extremities, however, most patients are asymptomatic. Longstanding hypocalcemia due to hypoparathyroidism can result in calcification of the basal ganglia and other intracerebral calcifications, cataracts, dermatological manifestations including dry, puffy skin, and coarse, brittle and sparse hair.
Hyperparathyroidism is a condition where the parathyroid produces too much hormone resulting in bone releasing calcium into the blood. This released calcium is a cause for osteoporosis and the elevated blood calcium leads to increased urinary excretion of calcium causing kidney stones. There can also be muscle, bone, and joint pain, and impairment of cognitive function.


is caused by a pituitary tumor that produces excess growth hormone (GH). It most commonly affects middle-aged adults and can result in serious illnesses or premature death.
is a growth or tumor on the pituitary that can put pressure on nearby structures, such as the nerves that connect the eyes to the brain, and cause symptoms. A large adenoma can also obstruct normal pituitary cells and keep them from working properly, leading to a condition called hypopituitarism. This condition can cause low blood pressure, tiredness, and changes in your sex drive and function. It can also make you feel less able to manage stress.
is a condition due to the primary hypersecretion of pituitary hormones, it typically results from a pituitary adenoma
are benign tumors of the pituitary gland that produce excessive amounts of the hormone prolactin. Prolactinomas are most common pituitary disorder, appearing in 50% of cases. In women, excess prolactin causes irregular or absent periods, inappropriate milk production, and infertility. In men, excess prolactin can cause sexual dysfunction and infertility. Symptoms can result from too much prolactin in the blood (hyperprolactinemia) or pressure from the tumor on surrounding tissues (if the tumor is large).
If the pituitary is not producing one or more of these hormones, the condition is called hypopituitarism. If all the hormones produced by the anterior pituitary are decreased, the condition is called panhypopituitarism. Hypopituitarism is most often caused by large benign tumors of the pituitary gland, or of the brain in the region of the hypothalamus.
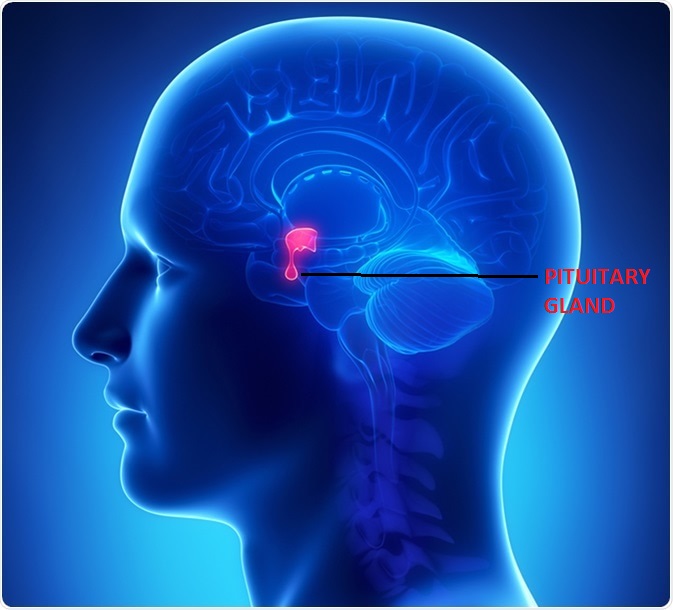



refers to a pituitary adenoma that produces excess ACTH, which stimulates cortisol secretion by the adrenal glands located above each kidney. Patients with Cushing’s disease have progressive weight gain, muscle weakness, easy skin bruising, impotence (in men), irregular periods (in women), and depression. Patients also have high blood pressure, diabetes, and osteoporosis. Many of these problems are non-specific.
is a disorder in which the adrenal glands do not produce enough of the hormones cortisol and aldosterone. Addison’s disease is caused by an autoimmune response, in which the body’s immune system assaults its own organs and tissues. Cortisol helps the body respond to stress, including the stress of illness, injury, or surgery. It also helps maintain blood pressure, heart function, the immune system, and blood glucose (sugar) levels. Aldosterone affects the balance of sodium and potassium in the blood, which in turn controls the amount of fluid the kidneys remove as urine, which affects blood volume and blood pressure
Diagnosing Lipid Disorders
Born Again Doctor Medical Center diagnose lipid disorders with blood tests and sometimes with additional imaging tests.
Lipids are waxy fats in the blood that are essential to a wide range of bodily functions. Cholesterol and triglycerides are two kinds of lipids.
Cholesterol is present in the cells of the body, and is a dietary component of non-plant foods. Triglycerides are also in the cells and in dietary fat, such as the white fat in meat, oils, and dairy products. The liver also produces cholesterol and triglycerides.
When the blood contains amounts of these substances that are outside of the healthy range—either too high or too low—this is known as a lipid disorder. People who have a high amount of certain lipids are at increased risk of developing cardiovascular disease.
Low-Density Lipoprotein
Low-density lipoprotein, known as LDL, or “bad,” cholesterol, is one of the most important components of your lipid profile. It circulates through your bloodstream and deposits cholesterol in your arteries. The cholesterol can accumulate and form plaques, which can lead to blockages that may cause a heart attack or stroke. Reducing your LDL through lifestyle changes and medications can help lower your risk.
High-Density Lipoprotein
High-density lipoprotein, or HDL—the “good” cholesterol—may help remove cholesterol from the body. A high level of HDL is associated with a reduced risk of cardiovascular disease. HDL levels are primarily influenced by genetic factors, but lifestyle changes such as tobacco cessation, weight loss, and exercise may be able to help you raise HDL levels.
Triglycerides
Triglycerides are fats that come from foods you’ve eaten and are present in your body’s cells. They are produced by the liver and fat tissue, especially when you consume excess calories, particularly from sugars and starches. The body carries triglycerides to tissues, where they provide energy or are stored, especially in fat tissue.
High levels of triglycerides have been linked to heart disease, as well as insulin resistance, type 2 diabetes, and obesity. Very high levels can also cause pancreatitis, an inflammation of the pancreas. Lifestyle changes, such as exercise, diet, and weight loss, can often help reduce triglyceride levels.
Causes and Symptoms
There are several different causes of lipid disorders. One of the most common is a genetic predisposition. Importantly, lifestyle habits can help decrease some of that risk—or worsen it.
A diet high in saturated fat, sugar, and simple carbohydrates can lead to increased lipid levels, especially triglycerides. Having increased belly fat is associated with elevated levels of LDL cholesterol, as well as high blood pressure and the risk of developing diabetes. People with diabetes, especially those who are sedentary, can also have disorders in which triglycerides accumulate in muscles or the liver, rather than being used as energy, which removes them from the body.
Taking certain medications, such as steroids, estrogen used in birth control pills, and certain medications to treat high blood pressure and psychiatric conditions, can increase lipid levels. Certain hormone disorders—including polycystic ovary syndrome (PCOS), hypothyroidism, and type 2 diabetes—can also result in high lipid levels.
A genetic disorder known as familial hypercholesterolemia, which begins in childhood, can cause chronically elevated cholesterol levels throughout a person’s lifetime. Levels may become so high that complications, such as a heart attack and stroke, can occur prematurely—even as early as the preschool years—if a person is not treated from a young age. Family members of people with the condition should be screened for it.
In the early stages of lipid disorders, there are no symptoms. High total cholesterol, high LDL, high triglycerides, and low HDL are often first detected in a routine blood test at an annual checkup. Some people with very high cholesterol and triglyceride levels may develop xanthomas—deposits of cholesterol that appear on the ankles or elbows—but this is not common.
Diagnostic Tests
To diagnose a lipid disorder, doctor checks your weight, since being overweight or obese is associated with elevated lipids, cardiovascular disease, and diabetes. Then, he or she may order one or more of the following tests.
Blood Test
Your doctor orders a blood test called a lipid profile. The test, which requires you to fast the night before, measures levels of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides—as well as other markers of health. LDL and HDL cholesterol measured on non-fasting blood are also accurate except in people with increased triglyceride levels, who may need a more specialized lipid test.
If your levels are elevated, your doctor may ask about your family history, diet, exercise habits, and other aspects of your lifestyle. He or she may perform further tests to rule out other causes of elevated lipids, such as thyroid disease, liver disease, kidney disease, and medications.
Lipid testing can give your doctor a sense of which foods you should avoid. If the results indicate that you have high levels of triglycerides, your physician is likely to recommend restricting refined carbohydrates, such as white rice and potatoes, as well as saturated and trans fats.
Advanced Lipid Testing
If your doctor wants to better understand your risk of a heart attack or stroke, and determine whether you might need intensive treatment, he or she may order advanced lipid testing.
During this test, your doctor checks your blood not just for levels of LDL and HDL, but for the number, or concentration, of these lipoproteins and their sizes. Some experts believe that this advanced assessment of lipoproteins is a more accurate predictor of cardiovascular disease then the basic lipid profile.
Coronary Calcium Score
To assess how a lipid disorder is affecting your health and whether you would benefit from treatment with medication, your doctor may order a coronary calcium score. This test involves a CT scan focused just on the area of the heart, and uses X-rays to assess the amount of calcium in your coronary arteries.
This exam enables your doctor to look for calcium deposits in the walls of your coronary arteries, which are an indication of the buildup of plaque that represents early coronary artery disease. A coronary calcium score has been shown to be an accurate reflection of a person’s risk of cardiovascular disease, and helps your doctor to determine how aggressively to treat a lipid disorder.
Carotid Intima-Media Thickness Test
A carotid intima-media thickness test is an ultrasound exam that allows the doctor to measure the amount of plaque in the neck arteries. This measurement gives your doctor an idea of how likely you are to develop cardiovascular disease.
The technician administering the test applies a thick gel to your neck, then moves a handheld device called a transducer up and down your neck. Sound waves bounce off the arteries in the neck, called the carotid arteries, and create images that are transmitted on a computer screen.
The test measures the thickness of the inner and middle layers of the arteries, the areas where cholesterol deposits first appear. An increase in the thickness of this region may be associated with higher risk of heart attack and stroke.
In addition, the amount of plaque in the neck arteries gives your doctor an idea of how much plaque may be in your coronary arteries. If a person has a large buildup of plaque, he or she may need more aggressive treatment to reduce his or her risk of heart attack and stroke